Imagine having painful knee arthritis so bad, or bone spurs limiting your range of motion, and you’re living in the 1800s. That’s a lot of limping. And think of now. Many procedures we take for granted such as knee replacement, or cataract surgery, treatments for GERD or gout, are now commonplace. Sit at a dinner table with a group of senior citizens and take a poll: how many have had joint replacement? There are currently almost 800,000 knee replacement surgeries performed annually, almost 600,000 hips.
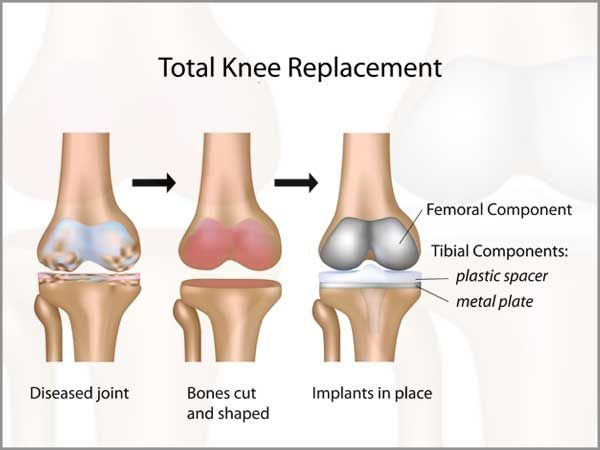
Knee replacement surgery has been around since 1890 when Dr Gluck used an ivory joint to replace a patient’s arthritic knee. Some surgeries were performed prior to this (1860s) to replace cartilage with no success. Imagine the pain and infections! Now TKR (Total Knee Replacement) is performed using robotic assistance. Times have changed, and so have I; I’m on my way to becoming the “6 million dollar woman” with my first (hopefully, last) TKR. This surgery has been expected for 27 years since I tore my ACL while skiing and further cartilage tears playing volleyball. Two arthroscopies and little to no cartilage later, I wore a metal brace for sports activities until the brace fell apart; by then, I didn’t need it much anyway because, age. Fast forward, bone-on-bone and many bone spurs later began causing discomfort and limited range of motion. While still mobile, I started getting cortisone injections to the knee-every 3 months for about 1.5 years. Most times they would eliminate pain for about 6-8 weeks (sometimes less). Time to get serious! I lost weight and got as active as was reasonable. Discussions with the local orthopedist centered around timing: there was no doubt I was “bone-on-bone” but pain was minimal; I could move and probably compensate enough to get around.n How does one volunteer for major surgery when not motivated by pain? Considerations we discussed: how long will the new joint last? What age might you be when it needs replacement? Might there be improvements in technology coming down the pike? No doubt, the situation would not improve so the decision was made to proceed and, to be scheduled at my convenience. Travel? Golf? I had a specific time window. Despite having a Sports Medicine group that treats Olympic athletes nearby, I opted to use a surgeon near Albany, Dr. Fred Fletcher. Dr. Fletcher was recommended by a friend and had impressive experience over his surgical career, which originated as a tech rep for a joint replacement manufacturer before med school. I was lucky to schedule prior to his retirement. In fact, I was his second to last surgery.
Pre-op appointments were required; blood tests, an Echocardiogram (not universally required), and approval from my PCP. Literature and information from the surgeon’s office was frequent and insistent. Timing the surgery was tricky: we were travelling through France in the 30 days leading up to the surgery and returned in just under the deadline for pre-op appointments. I also skipped the mandatory pre-op PT, doing the exercises on my own and getting fitted for the cane and walker by a PT friend. The final week pre-op I spent golfing and biking and house cleaning while the glorious fall weather persisted. If anyone has window washing secrets for streakfree results please, let me know.
For those of you considering TKR here are some specifics. No supplements or NSAIDs were allowed several days before surgery. No shaving either. I showered for each of the 4 days prior with Hibiclens as an infection preventative. Sheets were changed every night for a couple nights as well. The day of, no food after midnight the night before, and only minimal clear liquids and 8 oz of Gatorade 2 hr prior to arrival time. We drove the 3 hours to the surgical center. Once there, I was taken in, changed into a surgical gown, and wheeled into a pre-op room. The pre-op nurse inserted the IV line and cleaned my knee. The anesthesiologist, Dr. Haddad, came in to confirm my choice of anesthetic: a spinal nerve block and something to knock me out. I took some pills (ugh, can’t remember what) and then I waited about an hour and a half before the surgeon came in to check on me and confirm which knee he would operate on. I requested the lateral or “Jiffy” approach which leaves a scar to the side of the patella and not over the top. This method spares cutting the quad muscles, and allows for speedier recovery, but is more work for the surgeon. The beauty of using an experienced surgeon is having this option.

They were having a farewell lunch for Dr. Fletcher so it was pretty quiet for a bit after I was prepped. Hopefully, no champagne was served until later! All of a sudden a lot of medical personnel came in and by then I was woozy. Next thing I know, I’m in post-op with Greg by my side (Lowe’s and Harbor Freight errands completed). I dressed and walked up and down a few stairs and then we departed for our hotel. Yes, this was out-patient surgery, but they asked us to stay close in case of complications. I was at the surgical center a total of 4 hours; the actual TKR surgery takes only 1/2 hour. That night, I slept well (and probably still medicated) with my knee elevated and iced. The next morning we woke early, feeling good, buffeted on rubber eggs and yogurt for breakfast and drove home. There were no issues on the drive until we got within a mile or two of home; nausea had started. Our bumpy gravel road probably didn’t help.
Once home, I headed to the couch in our bedroom, accessing the second floor across the ledge and bridge, using a walker. There is such a distinct sound to walkers and canes; I hated it. To me, it reeks of infirmity. Anyway, a good friend had given me an ice machine which is basically an ice bath attached to a large cuff that wraps the knee and pumps ice water constantly. I remained knee-elevated and chilled for 2 days straight, day and night. I took the opioids (tramadol and oxycodone) as recommended for only 1.5 days; I was so nauseated I couldn’t stand it. I was also taking 1 g of Extra strength Tylenol every 6 hours, and 81 mg of aspirin and Celebrex every 12 hours, plus a stool softener. It took about 5 days for my digestive system to recover, which was likely the worst part of my immediate recovery. All this time I wondered when the spinal nerve block would wear off and the pain would start. I never felt any pain, just discomfort from the swelling and, of course, the nausea and gas.
The nausea ended once I went off the opioids. I began stretching as per their guidelines: simple leg raises and heel slides. Physical therapy began the third day after surgery. A few exercises at first: leg raises to strengthen my quads and assisted heel slides to stretch the quads-so painful! The knee was swollen, stiff, and tight. Third day in: I had 90deg flexion!

So many friends brought food and we were so grateful. Greg and I never touched the frozen meals I had pre-made. Family sent flowers too! Visitors kept me busy and happy and forced me to sit up and comb my hair. Thank you all!

By the end of the first week I had walked to the garage and we went out to dinner with friends. By 10 days I had doubled my distance/steps to about 2500 for the day. PT exercises were emphasizing stretching and strengthening. 12 days post surgery I returned to the surgeon’s office and the bandage was removed. The wound was closed so steri-strips replaced the waterproof bandage. The surgeon’s PA was pleased with my progress (107 deg flexion) and I was pronounced “no restrictions” and approved to drive. I went off the 1g/4x a day Tylenol, remaining on aspirin and Celebrex, Tylenol only as needed. Two weeks in I was walking 0.5 miles down the road and still working the PT exercises at home, punishing my quads 3 to 4x a day. My hamstrings were tight and rolling my muscles was more painful than the surgery. The lateral approach may slice fewer muscles but the surgeon had to manipulate them more, possibly resulting in my very sore legs. Also, apparently they use a tourniquet so that may account for some soreness. But, onward and upward! I started walking upstairs one stair per foot (down, however, still both feet each stair). At this point, Greg was released from nursemaid duty and life started getting back to normal. Not having been on the first floor for just over a week, I was curious to the effects of Greg’s cooking and homemaking. The kitchen was in great shape and the dishwasher emptied! Well done, honey! We got rid of the walker but I kept the cane handy for road walking but soon switched to trekking poles-strictly for safety. Stretching, strengthening, icing, and elevating continued, but for all intents and purposes, I was recovered and functioning again, 3 weeks in. The whole next week we were in Pennsylvania and my home-PT consisted of the recommended exercises but also ‘running’ around after twin toddler grandgirls, getting up and down off the floor, and rocking babies to sleep. Everyday was a full body workout but a mental and emotional slice of heaven.

Returning home I returned to official PT visits though toddler training helped me get to 117 deg flexion! At almost 4 weeks post surgery I was able to complete a revolution on the stationary bike, slowly and after having warmed up. Going downstairs required too much compensatory hip action so I was still taking each step with both feet. Knee swelling was down to 41 cm, compared to 36 cm on the ‘normal’ knee. And I was walking about a mile a day for exercise, in addition to the constant stretching and bending exercises that seemed to go on all day, with short icing and elevating stints in between. God bless those patients that got both knees done simultaneously! Double the heel slides-no way!!!
Four and a half weeks in, 120 deg flexion achieved and progress being made: almost ready to start walking downstairs normally (albeit slowly)! Now nearly off anti-inflammatories (Celebrex and aspirin) I’ve been able to enjoy a glass of wine occasionally. At 5 weeks post surgery: 125 deg flexion! (With warmup and pulling the heel in). 130 deg is the goal, with minimal effort. I was biking about 15 min daily in addition to the PT exercises which are all intended to stretch and strengthen hamstrings, quads, and glutes. Even my balance improved, and I started walking downstairs like a normal person, ever so slowly and carefully.

At 8 weeks post-op I realized I didn’t feel the stiffness that I had felt, like a compression band binding around the knee. Also, the numbness on the kneecap was subsiding. I still was taking stairs slowly, carefully bending my knee without hitching up my hip. Even that was just occasionally; if I overdid anything, stiffness due to swelling would set in and I’d have limited flexion for a bit until I rested the leg, preferably elevated with ice. Case in point: standing for almost 2 hours while making pierogi’s really caused stiffness to set in. What was still problematic: calf muscles were sore and raw, to the point of keeping me up or awakening me from sleep. I started massaging them nightly which seemed to help. And I was applying lotion or petroleum jelly to the scar and also massaging that too. But, I now had 126 deg flexion and 0 deg extension! (130 deg and 0 are the goals). To celebrate, I snowshoed almost 2 miles!

Notes and suggestions: -don’t wait too long to schedule surgery, if you need it. The healthier and more fit you go into it, the faster recovery will be. Yes, it’s a hassle. -I prepped frozen meals beforehand, tho neighbors brought enough food we never needed them. -I thought I’d lose weight but since food makes me feel better, nausea or no, that didn’t happen. Others have said they’ve lost weight. -I made lots of ice before and stored in the freezer, but we still needed to buy a few bags for the ice therapy machine. A suggestion from a friend: freeze those little short bottles of water instead and reuse. -I used the ice therapy machine exclusively the first few weeks (basically 24/7 the first few days even) but then switched to cold packs and frozen sleeves. -I found it hard knowing what was ‘too much’ when it came to exercise. When your knee is stiffer the next day, then it was too much, typically after an intensive PT session. -Elevate and ice, often. -I did PT exercises every day, about 30 min per session, 2x per day. -Sometimes muscles that weren’t affected directly by surgery will act up, like hips, calves, or glutes. Be sure to stretch or ice these too as they’ve been unworked or maybe you’re compensating. The whole leg is adapting. -Immediately begin working on bending and extension post-surgery. When elevating, the knee should be straight and above your heart. For extension, put your foot on a pillow, leg straight with nothing supporting your knee. Push down. -I joined a FB support group and saw that the TKR surgery results varied wildly. I unjoined. -Eat healthily; protein helps with healing. Get sleep. Drink water. Everything you should be doing anyway.

Epilogue: 15 weeks in, I do PT every morning for about an hour, then walk, bike, swim, or snowshoe later in the day. My swelling is down. My Range of Motion (ROM) is 130 deg (with coaxing). Recently, my physical therapist began focussing on loosening the tightness in my quads to achieve ROM using a torture device known as the Graston (?) technique, basically scraping the muscle to relieve tightness. Otherwise, except for some weakness in my hamstrings (working on it), I’m doing very well! I’ll be taking another 3 weeks off of PT appointments to travel (Egypt!), then will consider if that needs to be continued. I’m still impatient to be 100 %, but my therapist tells me to ‘hold my horses’ and that I am doing extremely well. Recommended recovery takes 6 months to a year, sometimes longer! I’ll take what I can get and continue focusing on strength. There’s lots of living to be done! I’m grateful, ever so grateful, for good health and good medical care.
